

22 Jun 2022 Clinical Documentation Improvement
What is Clinical Documentation Improvement (CDI)?
A CDI program is a process designed and implemented with the purpose of achieving accurate and thorough medical record documentation. Precise clinical documentation is integral to every patient encounter, as it assists providers to make informed decisions for patient care, helps assess the clinical quality, and determines appropriate reimbursement.
CDI programs have been a part of healthcare for a long. However, they got a boost in popularity around 2007 when the Centers for Medicare & Medicaid Services (CMS) implemented Medicare Severity Diagnosis Related Groups (MS-DRGs). Hospitals realized that accurate and thorough diagnosis code reporting increased reimbursement and reduced compliance risks. While CDI may have gotten its start in the inpatient environment, outpatient providers have recognized the benefit and started programs, as well. The primary focus of a CDI program for physicians in an office or outpatient environment is to help prevent these denials and amendments while also ensuring documentation is complete for clinical purposes.
The programs are usually undertaken by healthcare professionals with clinical and coding backgrounds, who undergo extensive training on the process. CDI specialists play a role in preparing providers and coders for coding and coverage changes and additional documentation requirements to accurately reflect the provider services and maximize reimbursements.
What does it include?
• Identification of potential issues associated with patient documentation such as those related to medical necessity and requirement of supporting documents at the same ensuring all conditions that are clinically supported are reported in the documentation.
• Reviewing of all relevant medical records including clinical notes, diagnostic exams, lab results, and prescriptions to assess for any inaccuracies within the patient’s documents, cause and effect relationship between conditions, or the possibility of any missed/under-coded diagnosis to ensure the level of service rendered is appropriately recorded.
• Making the provider aware of the importance of using more specific terms and including the status of all coexisting conditions being monitored or treated that affect medical decision-making in the documentation to ensure better patient outcomes, and data quality and prevent missing charges.
• Effective collaboration with the providers and coders to aid in streamlining the providers coding efforts, reducing errors and time needed by the coders.
Impact on reimbursement
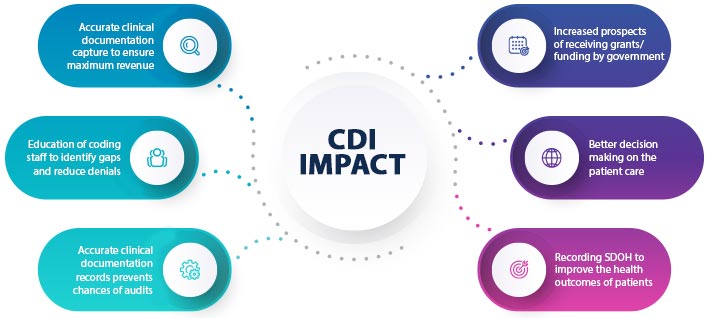
Nearly 90 percent of hospitals with 150 or more beds and outsourced clinical documentation functions realized at least $1.5 million inappropriate healthcare revenue and claims reimbursement following clinical documentation improvement (CDI) implementation, reported Black Book Market Research.
At CureMed Solutions, we provide the support and expertise needed to comprehensively assess patients’ documentation and also ensure that it is translated into accurately coded data enabling our clients to eliminate gaps in their documentation and improve reimbursement considerably.